I left at 6.30am as I had clinic attachments with Dr Deegan, my giant german consultant on the respiratory team. Despite his size, he moves pretty fast; his 6’6 frame ascending the stairs with surprising agility. I was out of breath by the time we reached the third floor. The clinic was full of people who presented with shortness of breath.
“We’re very lucky. Not one person who checked in this week is over 90,” said Deegan, aptly explaining the demographics of this small hospital. I could only smile at the irony.
Geriatrics is definitely out of the question. Old people just aren’t my forte. Getting a good history from an elderly person is almost impossible without getting into an hour long conversation about her grandkids or her recently dead dog. Not my cup of tea at all.
It’s always been paediatrics, but then again things may change in the years to come.
Advice?
Surgery
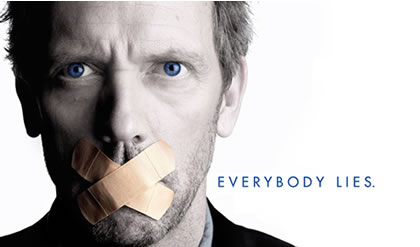
“Patients hate to see doctors who look like they don’t know what they’re doing. So even if you have no f***ing clue of what you’re doing, just look confident,” said Dr you-know-who.
I couldn’t agree more....
Cardiology
“First, learn to walk fast. Second, talk with a loud and clear voice. Third, look smart,” he continued much to our amusement.
Gynaecology
“I once landed in Saudi Arabia and they decided to check my laptop. They had me in for three hours because of all the vagina pictures. And then I became a gynaecologist,” joked O’ Heirlihy
The long road ahead..
It was almost 7pm. I wasn’t really tired. Just frustrated. It had been a long day.
“Why did you choose medicine?”
That question was asked almost 4 years ago. The interviewer must’ve liked my answer enough to have offered me a place in UCD.
I had only figured out a valid reason the night before, and I told them what they wanted to hear.
Again, that was four years ago...